View by group:
CURRENT STRATEGIC INITIATIVES
International Brain Initiative (IBI)
 The Declaration of Intent to establish the IBI was announced on 8 December 2017 at a meeting of representatives from some of the world’s major brain research projects, supported by The Kavli Foundation and hosted by the Australian Academy of Science in Canberra. The Declaration, made by representatives from Japan, S. Korea, Europe, the United States of America and Australia, is designed to speed up progress on ‘cracking the brain’s code’. Other member nations now include China, Canada, Finland, New Zealand, Africa, and Latin America.
The Declaration of Intent to establish the IBI was announced on 8 December 2017 at a meeting of representatives from some of the world’s major brain research projects, supported by The Kavli Foundation and hosted by the Australian Academy of Science in Canberra. The Declaration, made by representatives from Japan, S. Korea, Europe, the United States of America and Australia, is designed to speed up progress on ‘cracking the brain’s code’. Other member nations now include China, Canada, Finland, New Zealand, Africa, and Latin America.
As a convener for global neuroscience that is distinct from professional neuroscience societies or other institutions, today the IBI pursues its goals guided by the following vision and mission:
Vision: Border-free global science, scholarship, and innovation that are catalyzed by the critical engagement of large-scale brain initiatives and unprecedented opportunities for international collaboration, accelerating discovery research, and ensuring scientific advancements for the benefit of all people.
Mission: To provide a platform for active dialogue and exchange among large-scale brain initiatives worldwide, support the emergence of new initiatives, and catalyze collaboration on a global scale through priority scientific endeavours.
Aspirations
Transcend borders
-
- Between countries: Serve as a convener between IBI countries to promote involvement in the International Brain Initiative and enable synergistic interactions.
- Across research fields: Promote interdisciplinary perspectives and approaches to research and training to drive discovery and innovation.
- Among global citizens: Communicate transparently about the opportunities and challenges arising from the latest brain-inspired discoveries and innovation.
- With industry: Provide access to global engagement for the translation of discoveries.
Shape the future
-
- For international collaboration: Develop innovative and dynamic models for international research collaboration.
- For brain health: Foster a culture of scientific sharing and exchange about brain diseases on a global scale.
- For ethical practice in the brain sciences: Advance the highest standards of global ethical inquiry as an integral part of the global enterprise.
Canadian Brain Research Strategy (CBRS)
 The mission of CBRS is to build on Canada’s strengths and current investments in cutting-edge collaborative neuroscience to transform neurological and mental health for Canadians. The Strategy is a grass-roots initiative launched by leading Canadian neuroscientists, in partnership with representatives of the Neurological Health Charities of Canada to respond to a growing need for concerted efforts to understand the brain.
The mission of CBRS is to build on Canada’s strengths and current investments in cutting-edge collaborative neuroscience to transform neurological and mental health for Canadians. The Strategy is a grass-roots initiative launched by leading Canadian neuroscientists, in partnership with representatives of the Neurological Health Charities of Canada to respond to a growing need for concerted efforts to understand the brain.
Pan-Canadian Neurotechnology Ethics Collaboration
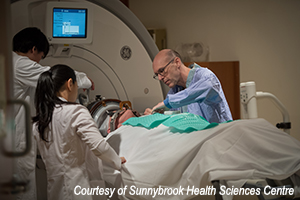 Groundbreaking work is being done in the areas of neurology and neurosurgery as new neurotechnologies open up the potential for innovative therapies for a variety of ailments of the brain, spanning psychiatric, neurodegenerative, and oncological disorders. However, the decision to make the transition from pre-clinical research to first-in-human trials is a difficult one, marked by the relative absence of information on the certainty of safety, efficacy, and risk of the intervention. While guidance exists for pharmaceutical development, there is less literature on this translation for novel surgical procedures and medical devices. Patients and practitioners alike are left with a dirth of tools to aid them in the decision to undergo a novel neurointervention. In the absence of such guidance, it is unclear what factors are the key drivers of decision makers’ choices. We seek to explore the factors that key stakeholders take into consideration when determining a novel neurointervention’s readiness for translation into first-in-human trials. Insight into the attributes of a novel intervention that drive patients’ decision making will allow clinicians and researchers to better understand patient values and preferences in future care and research. Similarly, insight into the factors that drive clinicians' and researchers' perceptions of readiness can inform the development and translation of future novel interventions for patients as well as regulatory guidance for the field. Our qualitative research will provide much needed data on the relatively underreported translational process for surgeries and novel medical devices.
Groundbreaking work is being done in the areas of neurology and neurosurgery as new neurotechnologies open up the potential for innovative therapies for a variety of ailments of the brain, spanning psychiatric, neurodegenerative, and oncological disorders. However, the decision to make the transition from pre-clinical research to first-in-human trials is a difficult one, marked by the relative absence of information on the certainty of safety, efficacy, and risk of the intervention. While guidance exists for pharmaceutical development, there is less literature on this translation for novel surgical procedures and medical devices. Patients and practitioners alike are left with a dirth of tools to aid them in the decision to undergo a novel neurointervention. In the absence of such guidance, it is unclear what factors are the key drivers of decision makers’ choices. We seek to explore the factors that key stakeholders take into consideration when determining a novel neurointervention’s readiness for translation into first-in-human trials. Insight into the attributes of a novel intervention that drive patients’ decision making will allow clinicians and researchers to better understand patient values and preferences in future care and research. Similarly, insight into the factors that drive clinicians' and researchers' perceptions of readiness can inform the development and translation of future novel interventions for patients as well as regulatory guidance for the field. Our qualitative research will provide much needed data on the relatively underreported translational process for surgeries and novel medical devices.
Funding Agency: Sunnybrook Research Institute
Bioethics Council of Canada
A self-directed Expert Group of leading ethicists in Canada has been working on a model for a legally-mandated, independent Bioethics Council to address national and international policy gaps and their significant implications to the health and well-being of Canadians and society.
A dedicated Bioethics Council for Canada, with weight acquired by virtue of the expertise of its members and a track record of providing timely, evidence-based and unbiased reports on bioethics questions, would be an invaluable advancement and resource for a new Canadian approach. Standing as an independent unit from government with expert representation across the territories and provinces, the Council would provide an organized and enduring readiness to support Ministerial priorities and be directly accessible to policy analysts to enable them to function optimally. Reports of the Council would not bind government; rather, they would strengthen democratic participation on issues of key importance to Canada by serving as a focal point for public discussion and debate.
Further readings:
- Opinion in The Conversation, 30 June, 2021:
https://theconversation.com/canadian-ethicists-recognize-the-critical-importance-of-science-and-research-163204 - Illes, J., Schaffrick, M., Ravitsky, V., Meslin, E.M., Bubela, T, Chandler, J.A., Knoppers, B.M., Upshur, R., Re-invigorating notions of a bioethics council for Canada in a new era of biomedicine, Kaleidoscope on Global Bioethics, 2023, [Maria do Céu Patrão Neves, Ed.], pp. 95-104.
CURRENT RESEARCH
International Neuroethics Patent Initiative (INPI)
In collaboration with colleagues at the University of Bonn, Centre for the Law of Life Sciences, in Germany, we are undertaking a multinational collaboration to examine neuroscience patents and the protection of intellectual property as they pertain to brain health and disease.
The abstract of the project is as follows:
Patents granted in the field of neuroscience cover diverse areas of diagnostics, devices, data processing methods and computational models, and networks and systems related to the central nervous system. Historically, patent protections have safeguarded the intellectual property of creative neuroscience discoverers and inventors, and offered financial incentives for innovation. Today, however, the far-ranging scope of neuroscience patents may lead not only to obstacles to research, but to massive threats to personal rights, human dignity, and health data protection. Compounding this threat are notions about “mind reading” and "the transparent brain" arising from new capabilities of both invasive and non-invasive brain computer interfaces (BCIs) involving signal recording and regional tissue stimulation variously in healthy individuals, and patients with neurological and psychiatric disorders. Here we propose to use methods from legal scholarship and the social sciences to: (1) examine patents already granted, (2) classify them into the applicable patent law, (3) address the question of the viability of the patent law that applies to them, (4) elucidate perspectives about the desirability and pitfalls of patents pertaining to brain from neuroscientists, patent lawyers, and patent officers, and other expert informants, and (5) close identified gaps that are unfulfilled and may place individuals, patients and society at risk. The limited discourse to date on brain patents is thus extended fully through this work and will, above all, be brought into patent law and policy decision-making.
Mend the Gap
Mend the Gap is an international effort devoted to developing a novel treatment for spinal cord injury that uses nerve regeneration. Key to its success is collaboration with the SCI community and an understanding of translation pathways, commercialization, and regulatory steps. As lead of the Ethics, Knowledge Translation and Patient Engagement arm of this effort, Dr. Judy Illes and her team will engage with individuals and stakeholders touched by SCI in new research to understand their values, perspectives, and priorities. The goal is to interface closely with the basic science teams and create models and tools for developing and communicating new treatments in a way that respects the heterogeneity of spinal cord injury, cultural and personal diversity, and autonomy.
For more information about Mend the Gap, please visit: https://mendthegap.ubc.ca/.
Crosscultural perspectives on mind and brain
The integration of Indigenous perspectives and knowledge with biomedical approaches in the neurosciences can significantly broaden the understanding of the human brain and mind. Drawing upon the writings of Elders in Canada, this integration is referred as Two-Eyed seeing or Etuaptmumk. In the upcoming Nature article (see details below), authors discuss how Two-Eyed Seeing and other dual perspectives can bring both breadth of knowledge and humility to the development of research and clinical practices for brain health. They include in this forward-looking discussion both traditional academic and non-academic traditions, and the work of Indigenous scholars on methodologies, life, health, culture, language, and history. To describe challenges and consider solutions, authors consider broad strategies for allyship, humility, and universalism, and situate them in four specific examples pertaining to disability, suicide, migration, and the environment. They further advance the power of Two-Eyed Seeing in the context of new considerations for communication and public engagement today. Two-Eyed Seeing, per se, is only one approach, but as neuroscience becomes ever more global, inclusive and ethically proactive, it must universally see the world of brain and mental health through the eyes of both reductionism and holism.
Further information may be found in the upcoming article:
Illes, J., Perreault, M.L., Bassil, K., Taylor-Bragge, R.L, Bjaalie, J.,G. Chneiweiss, H., Gregory, T.R., Kumar, B., Matashabe, O.P., Svalastog, A-L, Velarde, M.L. Two-Eyed Seeing and other Indigenous perspectives for neuroscience, Invited Perspective, Nature, in press.
Neuroprognostication After Opioid Overdose (NeuroPOD)
Addressing gender disparities in patent law
This project aims to use theoretical and empirical research to generate rich descriptions of alternative knowledge generation and governance systems. Empirical research will be grounded in critical feminist and queer intellectual property and technosicences frameworks, and will seek to create and spark conversations with gender diverse individuals on topics related to knowledge, creation, sharing, creativity, ownership, property and regulation. This project is lead by doctoral student Margot Gunning under the primary supervision of Dr. Graham Reynolds at the Peter A. Allard School of Law.
Ethical considerations of using neurotechnologies to treat opioid use disorder
Co-creating an Outcome Measure For social RoboTs in dementia care (COMFORT)
Social robots have the potential to improve independence and quality of life for persons living with dementia and their care partners. Although these devices are being deployed in many age-related contexts, tools that measure the impact of social robots in dementia care are lacking. This makes it difficult to determine whether social robots are truly useful and to compare between different devices. The COMFORT project will develop a validated outcome measure that will inform best practices and policies for social robot use in dementia care.
Funding Agency: Alzheimer’s Association
Self-disclosure about dementia on social media: Toward evidence- informed guidance
This project aims to understand the motivations and impacts of disclosing a personal dementia diagnosis or identifying as a care partner on social media.
Funding Agency: Alzheimer’s Association
Self-disclosure of mental illness on social media
Social media plays a significant role in the lives of children and adolescents, and exploring their online behaviours is critical to understanding overall youth developmental and mental health. Given that the self-disclosure of mental health information online is a newly popular phenomenon, this study aims to characterize the risks and benefits of its use among young people.
Funding Agency: BC Children’s Research Institute’s Brain, Behaviour, and Development Theme
Intergenerational determinants of social robot usability
Given the increasing development and use of social robots across the lifespan, this project aims to investigate key usability factors for social robots in children, adults and older adults and determine how goals and methods of interaction change over the lifespan and in different group contexts.
Co-creating an ethical framework for social media use in prevention trials
This project's research team aims to co-create guidelines that address the risks and benefits of social media use in dementia research. The goal of this project is to help researchers and participants connect on social media in a way that is ethical and beneficial for all.
Why is this research important?
Dementia research is still receiving limited engagement and low enrolment numbers, especially in diverse populations. Social media offers new ways to overcome geographical and financial barriers and can increase awareness of important dementia research.
The aim of this research study is to co-create practical guidelines for researchers using social media in prevention trials.
For more details on this project, please visit: https://www.nestlab.ca/co-creating-an-ethical-framework-for-social-media-use-in-prevention-trials.html
Social Co-creation of Robotic Assistive Technologies (SOCRATES)
Funding Agency: Canada’s Tri-Council Agencies (SSHRC)